Achondroplasia
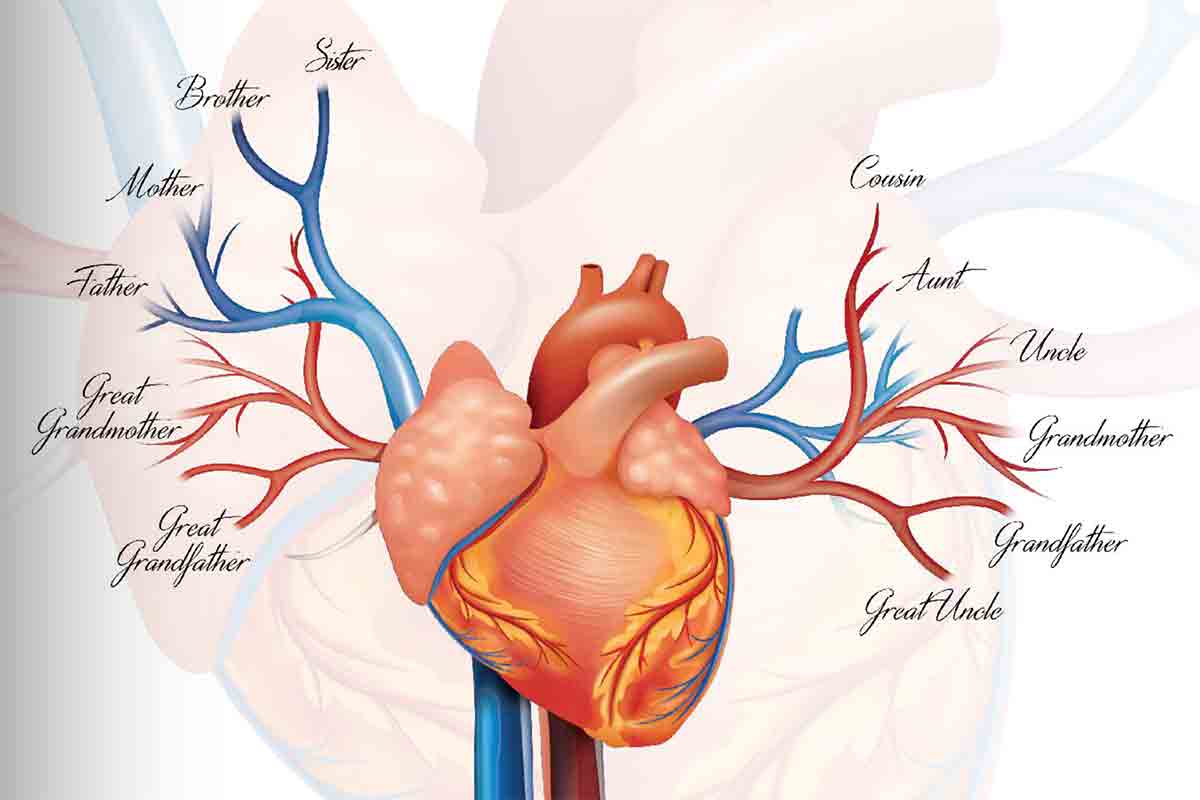 Image courtesy of American College of Cardiology Opens in new window
Image courtesy of American College of Cardiology Opens in new windowImage is that of familial hypercholesterolemia
Achondroplasia is incompletely dominant skeletal disorder of short-limbed dwarfism and large head. Most achondroplastic individuals have normal intelligence and lead normal lives within their physical capabilities. Marriages between two achondroplastic individuals are not uncommon. A homozygous child of two heterozygotes is often recognizable on clinical grounds alone; individuals homozygous for achondroplasia are much more severely affected than are heterozygotes and commonly do not survive the immediate postnatal period.
FH is characterized by isolated elevation of plasmatic low-density lipoprotein (LDL) cholesterol and premature coronary artery disease (CAD), is associated with mutations in three major genes: LDL receptor (LDLR), apolipoprotein B (APOB) and proprotein convertase subtilisin/kexin 9 (PCSK9).
Homozygous patients have rapid development of atherosclerosis with death from cardiovascular disease even in childhood.
Clinical Features and Expression
Homozygous FH is caused by the inheritance of two mutant genes at the LDL receptor locus.
The clinical expression occurs in approximately 1 in 1 million persons.
The defect in LDL receptor function causes a marked elevation in the plasma concentration of LDL-C, which typically exceeds 500 mg/dL but can reach as high as 1000 mg/dL. HDL cholesterol (HDL-C) concentrations tend to be substantially below normal.
Clinical features include the presence of xanthomas, severe aortic root disease including aortic stenosis, and the premature onset of coronary artery disease (CAD). Angina pectoris, myocardial infarction, or sudden death frequently occurs between the ages of 5 and 20 years.
Mabuchi et al. followed 10 patients with homozygous FH for a period of approximately 14 years. During that time, six of the patients died from sudden death or heart failure at an average age of 26. Similar observations were reported in patients from South Africa.
The severity of the clinical expression depends to a great extent on the percentage of functioning LDL receptors.
In the study by Goldstein and Brown of 57 homozygotes, more than one fourth of receptor-absent patients died before the age of 25 compared with 1 of 26 individuals with residual LDL receptor activity. Because of the very high risk of premature coronary artery disease (CAD) and the poor response to diet and drug therapy, all patients with homozygous FH require alternative therapy.
Patients with Low-Density Lipoprotein Cholesterol Concentrations of More Than 200 mg/dL and Coronary Artery Disease
The majority of patients in this group will have the heterozygous form of FH, heterozygous familial hypercholesterolemia (HeFH) . This disorder has a prevalence of approximately 1 in 500 persons and is typically manifested by the occurrence of premature coronary artery disease (CAD) by the fifth decade for men and the sixth decade for women.
Clinically similar syndromes are produced by defects in the LDL receptor and defective apolipoprotein B (apoB) structure with impaired receptor binding.
The presence of both CAD and elevated LDL concentrations is an important risk factor for subsequent coronary events, and therefore patients with CAD require intensive LDL-C concentration control.
The reinfarction rate found in seven secondary prevention trials reviewed by Pekkanen et al. was about 6% annually in contrast to a 1% rate of first infarction in four primary prevention trials.
Trials in patients with marked hypercholesterolemia have reported regression or a lower rate of progression of coronary lesions when the elevated LDL-C concentration is lowered with diet and drugs.
Coupled with the impressive results from the trials that used the statins, a very persuasive case can be made for the aggressive treatment of subjects with familial hypercholesterolemia to achieve NCEP LDL-C targets.
Management
Since heterozygous familial hypercholesterolemia (HeFH) is a disease that exposes the individual from birth onwards to severe hypercholesterolemia with the development of early cardiovascular disease, a clear consensus on the management of this disease in young patients is necessary.
In Belgium, a panel of pediatricians, specialists in (adult) lipid management, general practitioners and representatives of the FH patient organization agreed on the following common recommendations.
- Screening for HeFH should be performed only in children older than 2 years when HeFH has been identified or is suspected (based on a genetic test or clinical criteria) in one parent.
- The diagnostic procedure includes, as a first step, the establishment of a clear diagnosis of HeFH in one of the parents. If this precondition is satisfied, a low-density-lipoprotein cholesterol (LDL-C) level above 3.5 mmol/L (135 mg/dL) in the suspected child is predictive for differentiating affected from non-affected children.
- A low saturated fat and low cholesterol diet should be started after 2 years, under the supervision of a dietician or nutritionist.
- The pharmacological treatment, using statins as first line drugs, should usually be started after 10 years if LDL-C levels remain above 5 mmol/L (190 mg/dL), or above 4 mmol/L (160 mg/dL) in the presence of a causative mutation, a family history of early cardiovascular disease or severe risk factors.
The objective is to reduce LDL-C by at least 30% between 10 and 14 years and, therefore after, to reach LDL-C levels of less than 3.4 mmol/L (130 mg/dL) (O. S. Descamps et al., Brussels Free University).
Patients with Low-Density Lipoprotein Cholesterol Concentrations of More Than 300 mg/dL without Coronary Artery Disease
The decision of whether to use nondietary, nondrug therapy for primary prevention in asymptomatic adults is never as easy as it is in homozygotes.
The risk of premature CAD is most apparent in patients with FH due to the presence of life-long elevated LDL-C concentrations. In addition the presence of risk factors other than LDL-C helps determine which patients are most likely to develop CAD.
For example, a lipoprotein(a) [Lp(a)] concentration of more than 20 mg/dL has been recognized as an independent risk factor in patients with FH.
The use of noninvasive screening procedures for CAD, such as quantitation of coronary artery calcium, provides additional guidance for determining whether patients with elevated LDL-C will develop clinically significant disease.
Based on current FDA guidelines, it is reasonable to consider nondietary, nondrug therapy for primary prevention in patients with an LDL-C concentration of more than 300 mg/dL despite diet and maximal tolerated lipid-lowering drug therapy.
See also:
- Adapted from:
- Familial Hypercholesterolemia: New Insights for the Healthcare Professional, 2012 Edition.
- Cardiovascular Therapeutics: A Companion to Braunwald's Heart Disease by Elliott M. Antman

