Family History
Definition and Importance
The family history consists of medical information about disorders that are present or have occurred in the patient and direct blood relatives of the patient.
Psychosocial information (relationships, demographics, occupation, behavioral factors, and environmental factors) is also collected as part of the family history.
This information can help the provider identify any predisposition to illnesses and enable education and prevention strategies to avoid behavioral and environmental triggers.
Family history, particularly when presented as a three-generation pedigree Opens in new window, is one of the most important indicators of disease risk currently available and is an important component of the Essential Genetic and Genomic Competencies for Nurses. Even more so is family history important to obtaining an accurate genomic assessment.
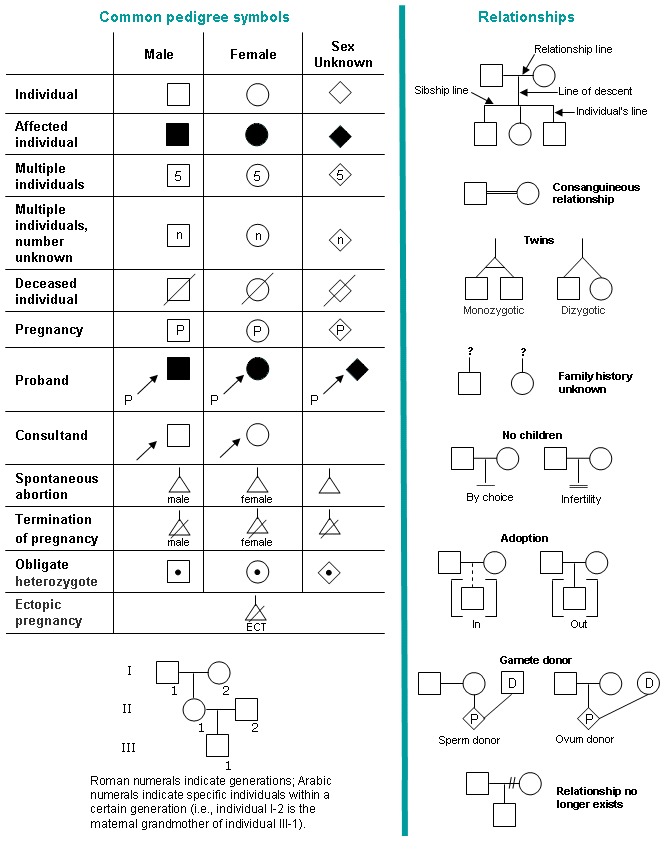
| Table X-1 | Standardized Pedigree Symbols and Relationship Lines Commonly Used in Family History. |
|---|
|
In the future, it is likely that medical and family history will be used to help the clinician better understand variants and their penetrance Opens in new window within the family and individual with a disorder.
Notably, the family history is a cost-effective approach to health care that can be used to initiate health interventions. Whenever possible, this information should be recorded in the form of a three-generation pedigree Opens in new window, using standardized symbols, as displayed in Table X-1, so that interpretation is consistent across heath care professionals (HCPs) and practices.
Use of a three-generation pedigree Opens in new window when conducting a family history provides a depiction of family members by sex, across generations (e.g., three generations), enabling visualization of patterns and traits that cluster around the family.
This depiction provides useful information in determining Mendelian patterns of inheritance Opens in new window associated with hereditary disorders, as well as enabling health care professionals (HCPs) to begin to assess risk for disease; identifies at-risk family members; distinguishes genetic from other risk factors, and aids HCPs in making care and surveillance management decisions (Bennett, 2010).
Further, the pedigree Opens in new window provides a means for risk assessment and can serve to identify medical screening needs for healthy individuals.
The use of the pedigree also aids in establishing client rapport and decision-making and is useful in clarifying client’s misconceptions. Thus, the family history serves not only as a valuable diagnostic tool but also an important educational tool.
Importance of Family History Across Clinical Settings
The type of clinical setting and situation may influence the family history information collected and the application of the family history.
Although it is the hope that every individual will have a comprehensive three-generation pedigree Opens in new window as part of his or her medical record that is updated regularly, certain clinical settings may require a more focused approach to the family history.
For example, a preoperative screening would require a targeted approach focusing on risk due to complications that can occur during surgery (e.g., a family history of blood clots or bleeding disorders) and with anesthesia.
A preconception counseling or prenatal clinic visit, however, requires an in-depth family history to identify patterns in the family that may be suggestive of potential single gene disorders warranting possible genetic screening and counseling.
A family history is also essential in primary care and specialized clinic settings (e.g., internal medicine, cardiology) to determine risk for disease, early diagnosis, and personalized/precision management of care.
In fact, the Surgeon General, in cooperation with other agencies with the U.S. Department of Health and Human Services, launched a national public health campaign called the Surgeon General’s Family History Initiative, to encourage all American families to learn more about their family health history (National Human Genome Research Institute, 2012).
It is up to heath care professionals (HCPs) to ensure that this family history is incorporated into the medical record and updated during the individual’s clinic or hospital visit.
Regardless of the setting, genomic principles such as a the pedigree collection need to be put into practice and integrated across clinical situations (Greco et al., 2012).
Incorporating the information is important since family history is often referred to as the first genetic test, because it is used to guide the diagnosis of presymptomatic Opens in new window individuals with a genetic disorder (single gene) who may warrant further diagnostic or genetic testing or referral to specialists for management of care.
For common complex disorders (e.g., diabetes, hypertension), family history informs individuals about needed screening, testing, and targeted interventions for prevention, early treatment, and education.
Family history also helps the clinician build rapport with the patient to identify the shared environment and behaviors that might place the individual at higher risk for disease.
The Centers for Medicare and Medicaid Services determined that the family history is a crucial component of the physical examination visit and is required for reimbursement of the patient encounter (Department of Health and Human Services/Centers for Medicare and Medicaid Services, 2010).
Family history is an essential tool to be used throughout the life span and in specialized settings.
In the prenatal clinical setting, assessment often focuses on single gene disorders, chromosomal abnormalities, congenital malformations or other genomic conditions, in which, based on the family history or other information, a myriad of invasive and/or noninvasive procedures (e.g., chronic villus sampling, maternal serum alpha fetal protein, ultrasound) may be warranted for appropriates and early prenatal diagnosis.
Family history during the prenatal visit not only assesses genetic risk to the offspring, but also establishes disease carrier status of the parents. Once a parent is identified as a carrier of a genetic disorder (e.g., sickle cell Opens in new window, cystic fibrosis Opens in new window), this becomes useful data in determining disease risk to the newborn and determining other at-risk family members. The information is also important for reproductive counseling and family planning.
Multiple birth defects are often associated with chromosome abnormalities, particularly where there is a family history of miscarriages, infertility, mental disability, or delay, all of which are important to record on the family history, including the pedigree Opens in new window.
Further, newborn screening at time of the infant’s birth provides an array of measures to detect potentially fatal or disabling conditions in newborns due to single gene disorders, and the family history may provide additional information to aid in obtaining these screening tests.
Whole genome and other sequencing strategies during the newborn phase, in addition to the family history, may identify important information for future health care needs.
During the pediatric visit, family history guides the diagnosis of both single gene disorders and common chronic conditions.
Many single gene disorders first become evident during childhood, and common chronic diseases that run in families often have preclinical signs in children and adolescents.
For example, children with a strong family history of coronary artery disease may show early signs of atherosclerosis, such as elevated markers for inflammation and high cholesterol level.
Family history is useful in the adult health care setting for diagnosing adult onset single gene disorders (e.g., hemochromatosis, Huntington disease Opens in new window) and common chronic disease predisposition (e.g., genomic disorders) that have complex etiology, such as cancer, cardiovascular disease, hyperlipidemia, and diabetes.
The bulk of family history in the adult primary care setting focuses on the genomics of common chronic diseases, which is becoming increasingly important in the era of personalized healthcare (Chen et al., 2014).
The collection of the family history in this age group can be used to motivate patients to make healthier life style choices and undergo recommended screenings for disease prevention and health promotion.
Evidence from the United States Preventive Services Task Force (2011) found the family history is an important clinical consideration for issuing screening and prevention recommendations for breast cancer, colorectal cancer, lipid disorders, coronary heart disease, and abdominal aortic aneurysm.
Although single gene disorders in the general population are rare, the family history is critical to identification of the rare, single gene cancer syndromes and other single gene etiologies that often present in adulthood, in order to refer these high risk individuals for the proper disease management and in some cases disease prevention.
Utilization of the family history in the acute care setting assumes an important role in safety of the hospitalized patient. A family history of blood clots (e.g., Factor V Leiden) can require aggressive interventions for the patient undergoing surgical procedures.
Dosing and medication choice, for example, warfarin for deep venous thrombosis, may require pharmacogenomic testing for proper disease management for individuals carrying the specific polymorphisms for Factor V Leiden.
A family history of malignant hyperthermia, a potentially fatal pharmacogenomic disease, is triggered by several anesthetics and should always be included as part of the perioperative family history.
Although the settings differ, these scenarios underscore the importance of the personal Opens in new window and family history. Many of the previous examples focused on single gene disorders, which cannot be ignored but are rare in the general population.
As science moves into the genomic era, the family history is still considered very important as a screening tool for chronic disease, behavioral and environmental risks, as well as a potential aid in pharmacogenomics and disease management.
- Adapted from: Genomic Essentials for Graduate edited by Diane C. Seibert, Quannetta T. Edwards, Ann H. Maradiegue, Susan T. Tinley

